A PET/MR scan – what does it look like, what can it reveal and how should I prepare for it?
A PET/MR scan, which combines positron emission tomography with magnetic resonance imaging, is one of the most advanced diagnostic techniques available in modern medicine. It provides an accurate picture of body structures and metabolic processes, which is essential for the detection, diagnosis and monitoring of a wide range of diseases, particularly in the fields of oncology, neurology and cardiology. What does this innovative examination look like? What can it reveal and how should the patient prepare?
What is positron emission tomography?
Positron emission tomography (PET) is an innovative diagnostic technique that detects radiation emitted by radioactive substances that are introduced into the body. As a molecular imaging technique, PET uses positron-labelled tracers that accumulate in tissues and allow their metabolic function to be assessed. It is extremely effective at detecting even subtle lesions in tissues, including those associated with cancer.
The PET technique is particularly useful in oncological diagnostics, as it allows early detection of tumours and assessment of their spread and response to treatment. PET can also be used to assess the state of the heart and brain, enabling cardiological and neurological diagnostics. Most importantly, it is a valuable tool for planning treatment and monitoring the effects of treatment.
What is a PET/MR scan?
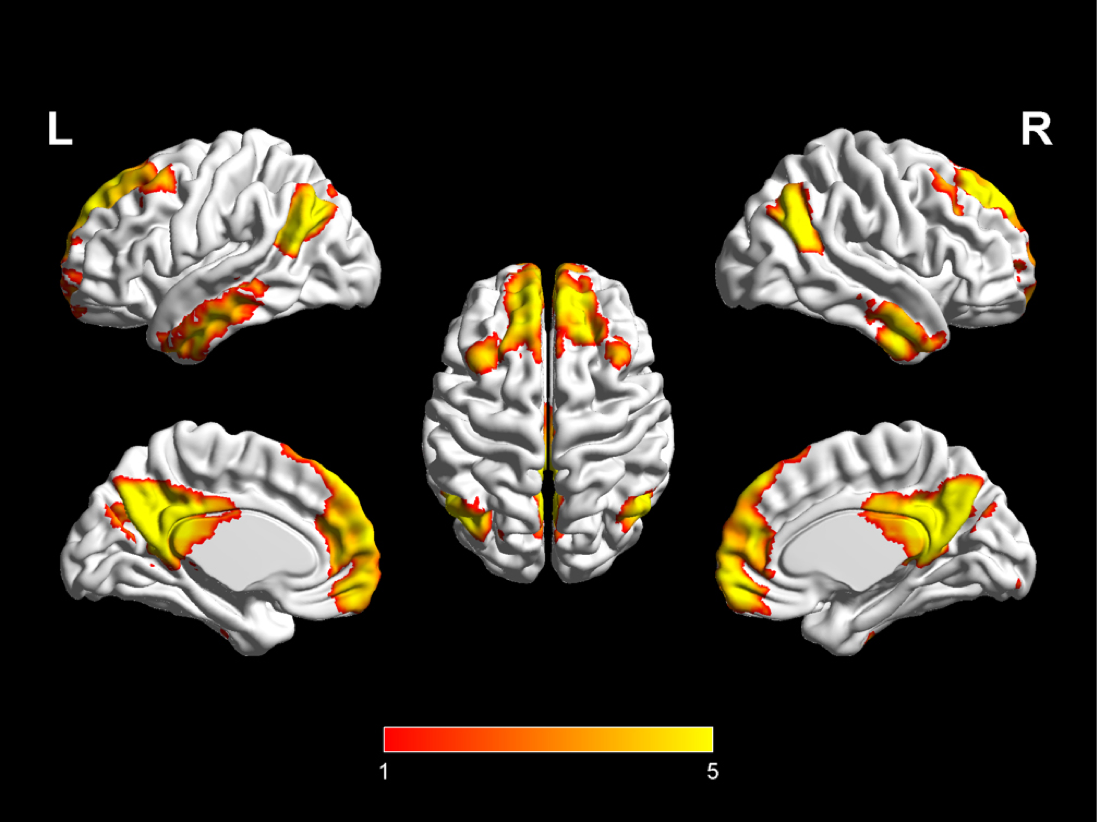
PET/MR combines the advantages of positron emission tomography (PET) and magnetic resonance imaging (MRI) to give doctors a comprehensive picture of a patient’s health. PET provides information about the function of cells and tissues, while MR provides an accurate picture of their structure. The combination of these two techniques allows for a more accurate diagnosis of various conditions, particularly cancer, heart disease and brain disease.
PET/MR scans are particularly useful in oncological diagnostics, allowing the precise localisation of tumours and the monitoring of their response to treatment. In neurology, this imaging modality is used to diagnose and monitor neurodegenerative diseases and to assess brain function. In cardiology, PET/MR can be used to assess myocardial viability and blood flow.
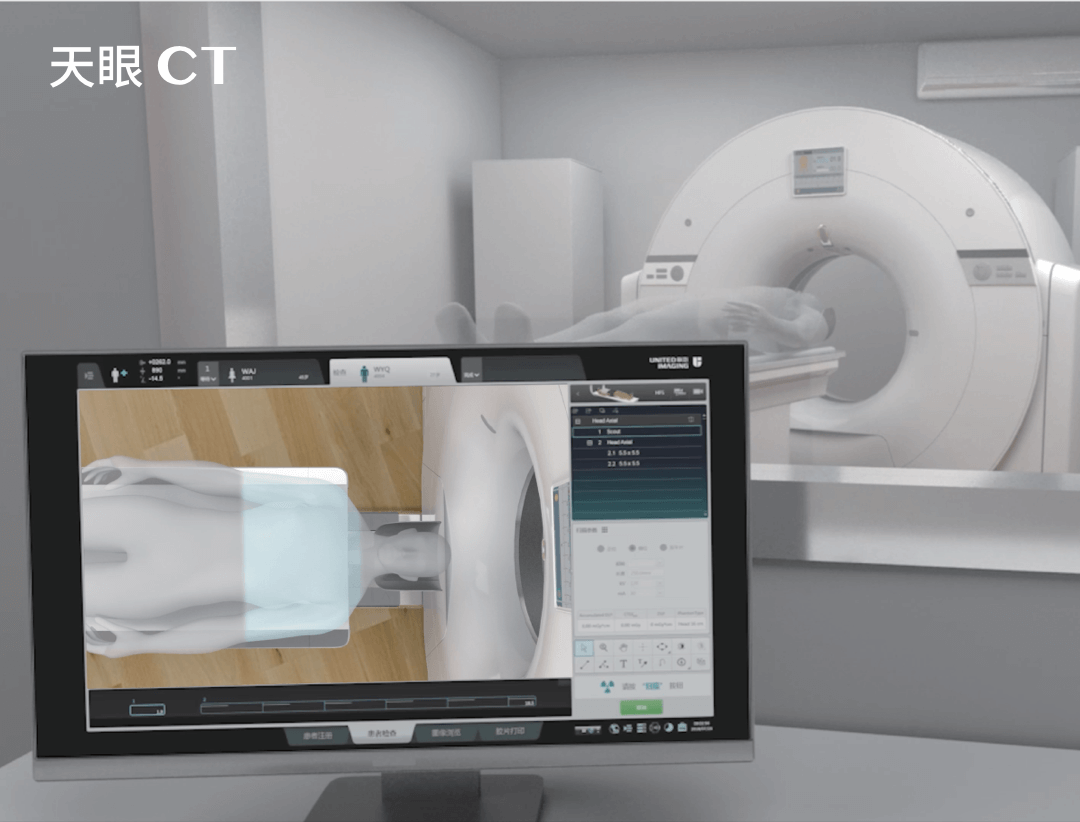
PET/MR equipment
PET/MR scanners incorporate advanced technologies that allow both examinations to be performed simultaneously. These machines combine PET detectors, which record positron emissions, with MR magnets, which allow anatomical structures to be imaged. This makes it possible to obtain metabolic and anatomical images at the same time, improving diagnostic accuracy.
There are many advantages to integrating PET and MR in a single unit, the most important being:
- reduced scan time, as both examination techniques are performed simultaneously;
- more consistent and accurate data, which is particularly important for complex oncological, neurological and cardiological diagnoses.
What can a PET/MR scan detect?
PET/MR is particularly useful in the detection and monitoring of cancer. This technique allows the metabolic activity of the tumour to be assessed, which is crucial in differentiating benign from malignant lesions. Additionally, PET/MR can be used to monitor the tumour’s response to treatment, which is essential for planning further therapy.
PET/MR can also be used to diagnose heart disease, including assessing myocardial blood flow and identifying damaged areas after a heart attack. In neurology, it is used to diagnose neurodegenerative diseases such as Alzheimer’s and to assess the effects of head injuries.
Is positron emission tomography combined with magnetic resonance imaging safe?
PET/MR is considered to be a safe diagnostic technique. This technique minimises the patient’s exposure to ionising radiation, which is present in conventional PET/CT scans. Magnetic resonance imaging, which is part of PET/MR, does not use X-rays, making it even safer.
However, like all diagnostic procedures, PET/MR has some limitations and risks. The most important of these are the use of contrast media and radioactive isotopes, which may be contraindicated in some patients. Therefore, an individual risk-benefit assessment is required in each case.
What does a PET/MR scan look like?
A PET/MR scan starts by injecting the patient with a radioisotope-labelled tracer, which accumulates in the tissues The patient then lies on a moving table that slides inside the PET/MR scanner. The patient must remain still during the scan to ensure the best possible image quality.
The PET/MR scan can take between 30 minutes and an hour, depending on the area of the body being scanned. During the scan, the patient is monitored by the operator who can communicate with the patient by intercom. After the scan, the patient can return to his or her normal activities.
How do I prepare for a PET/MR scan?
There are several important steps to preparing for a PET/MR scan. First, the patient should fast for at least 6 hours before the scan to ensure optimal conditions for radioisotope accumulation. The patient should also avoid strenuous exercise and alcohol consumption the day before the scan.
Patients should also inform the medical staff of any allergies, especially to contrast media, and of any medical conditions or medications they are taking. It is also a good idea to drink plenty of fluids before and after the scan, as this helps to clear the radioisotope from the body.
Contraindications to a PET/MR scan
There are some contraindications to a PET/MR scan, including pregnancy, breastfeeding, certain heart and kidney conditions, and the presence of metal or electronic implants that can interfere with MR imaging. In addition, patients with claustrophobia may require special care or preparation for the scan.
In all cases, the decision to have a PET/MR scan should be based on a thorough assessment of the patient’s health and consultation with a doctor. Despite some limitations, PET/MR is a valuable diagnostic tool that provides comprehensive information about a patient’s health, allowing more accurate treatment planning and monitoring.
*ATTENTION! The information contained in this article is for informational purposes and is not a substitute for professional medical advice. Each case should be evaluated individually by a doctor. Consult with him or her before making any health decisions.