Cephalometry – what is it?
Cephalometry is a specialist radiological examination that is essential in orthodontics and dentistry. As a tool that provides an accurate analysis of the facial skeleton, cephalometry is fundamental to planning effective orthodontic and dental treatment strategies. How does this work in practice?
What is cephalometry?
Cephalometry, also known as cephalometric radiography, is an advanced radiological technique that plays a key role in the evaluation of the facial skeleton, particularly in the diagnosis and treatment of malocclusions. This examination involves a detailed lateral radiograph of the skull, which allows a precise understanding of the relationship between the facial bones and an assessment of their growth dynamics.
Cephalometry in orthodontics and dentistry
Cephalometry is one of the basic examinations in orthodontics and dentistry that allows for the proper preparation of an orthodontic treatment plan. Cephalometry allows a precise analysis of an X-ray image of the skull in a lateral position, thus enabling the anatomical causes of malocclusions to be assessed.
Interestingly, the patient’s skeletal age is determined from of the cervical vertebrae visible on the photograph, which is very important for proper planning of the treatment process. The cephalometric photograph is also useful for monitoring the progress of orthodontic treatment already underway.
Cephalometry – not only for orthodontics
It is worth noting that cephalometry is not only used in orthodontics, but also in dental and ENT diagnostics, where it allows the width of the upper airway to be assessed. This tool is also used in reconstructive surgery and prosthodontics, giving doctors a detailed picture of the bones as well as soft and hard tissues of the face, hard palate and paranasal sinuses.
Indications and uses of cephalometry
Cephalometry is mainly used at the beginning and end of orthodontic treatment. Its main advantage is that it provides the exact measurements needed to prepare the correct braces. Cephalometry shows the relative positions of the skull, jaw and mandible and allows the direction of facial growth and changes resulting from the orthodontic treatment process to be determined.
Cephalometric images are taken using the latest technology, which reduces radiation exposure and minimises the risk of patient movement during the examination, thus improving the quality of the image produced. Using a cephalostat attachment, it is also possible to determine skeletal age in children, and obtain AP images of the skull and lateral images of the cervical spine.
Cephalometry versus radiography
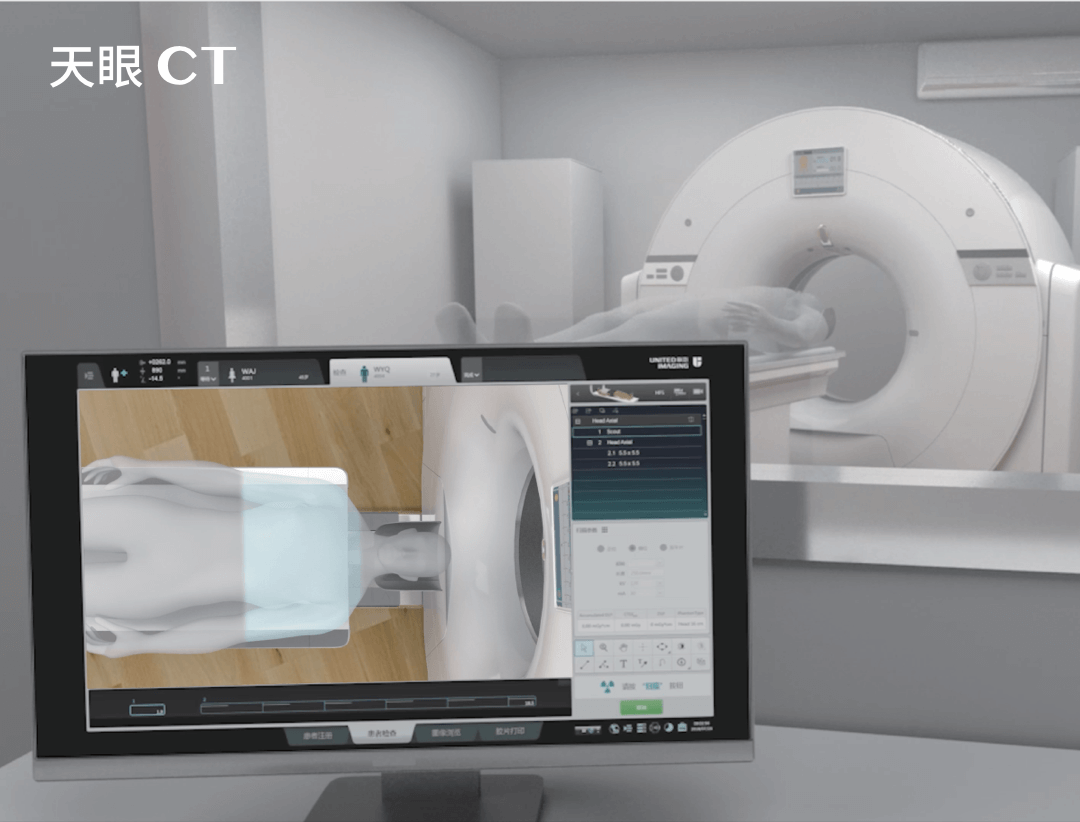
During a cephalometric examination, the patient is exposed to X-rays. However, using United Imaging Healthcare’s advanced diagnostic imaging equipment, the radiation dose is minimal, making the examination safe for the patient. It is often performed on children who need treatment for malocclusion, as accurate orthodontic diagnosis and rapid initiation of therapy are critical to achieving optimal results.
What a cephalometric examination looks like
The equipment used for cephalometry may be familiar to patients who have had pantomography. In order to take a cephalometric image, a special attachment must be fitted so that the patient’s head is held still during the examination, so that the image is readable and clear. The examination itself does not require any special preparation. However, the patient must remove any metal objects in the head and neck area, such as earrings, pins or pendants, just before the photograph is taken.
Referral for cephalometric examination
Similar to computed tomography (CT) scans or X-rays, a patient must have a current referral from a doctor in order to undergo a cephalometric examination. When a patient visits a doctor with a cephalometric scan, it is recommended that he or she bring any previous cephalometric scan results he or she may have had, as this will give the doctor a more complete picture of the patient’s medical history, making it easier to make the correct diagnosis and plan further treatment.
*ATTENTION! The information contained in this article is for informational purposes and is not a substitute for professional medical advice. Each case should be evaluated individually by a doctor. Consult with him or her before making any health decisions