MRI during pregnancy – safety, indications and contraindications
Magnetic resonance imaging (MRI) is among the most advanced medical imaging techniques, offering exceptional accuracy in diagnosing a variety of conditions, pathologies and injuries to the human body. Alongside these advantages, MRI is considered one of the safest diagnostic examinations. A question that often arises in the context of MRI is its use in pregnant women. During pregnancy, the health of the mother and of the developing foetus are a priority, and therefore any medical intervention requires special care.
Is a magnetic resonance scan during pregnancy safe?
Unlike imaging modalities such as X-rays and computed tomography (CT) scans, an MRI scanner does not emit ionising radiation that could pose a risk to the developing foetus, which is a key argument for its safety. According to the studies conducted to date, radio-frequency waves and the strong magnetic field used during MRI have not been demonstrated to have any negative effects on foetal health. Nevertheless, it is standard practice to avoid performing MRI in the first trimester of pregnancy unless there are compelling medical indications to do so. The examination is considered safer in the second and third trimesters when the foetal organs have already developed.
Indications for MRI in pregnancy
The most common examination performed in pregnant women is ultrasound, but in some cases this does not provide sufficient information to make the precise diagnosis necessary to ensure the health of the mother or of the foetus. In such cases, an MRI scan is performed, which enables more detailed images to be obtained. This is particularly recommended in the following cases:
- amniotic fluid volume disorders, such as oligohydramnios or polyhydramnios, where proper assessment of amniotic fluid volume is crucial;
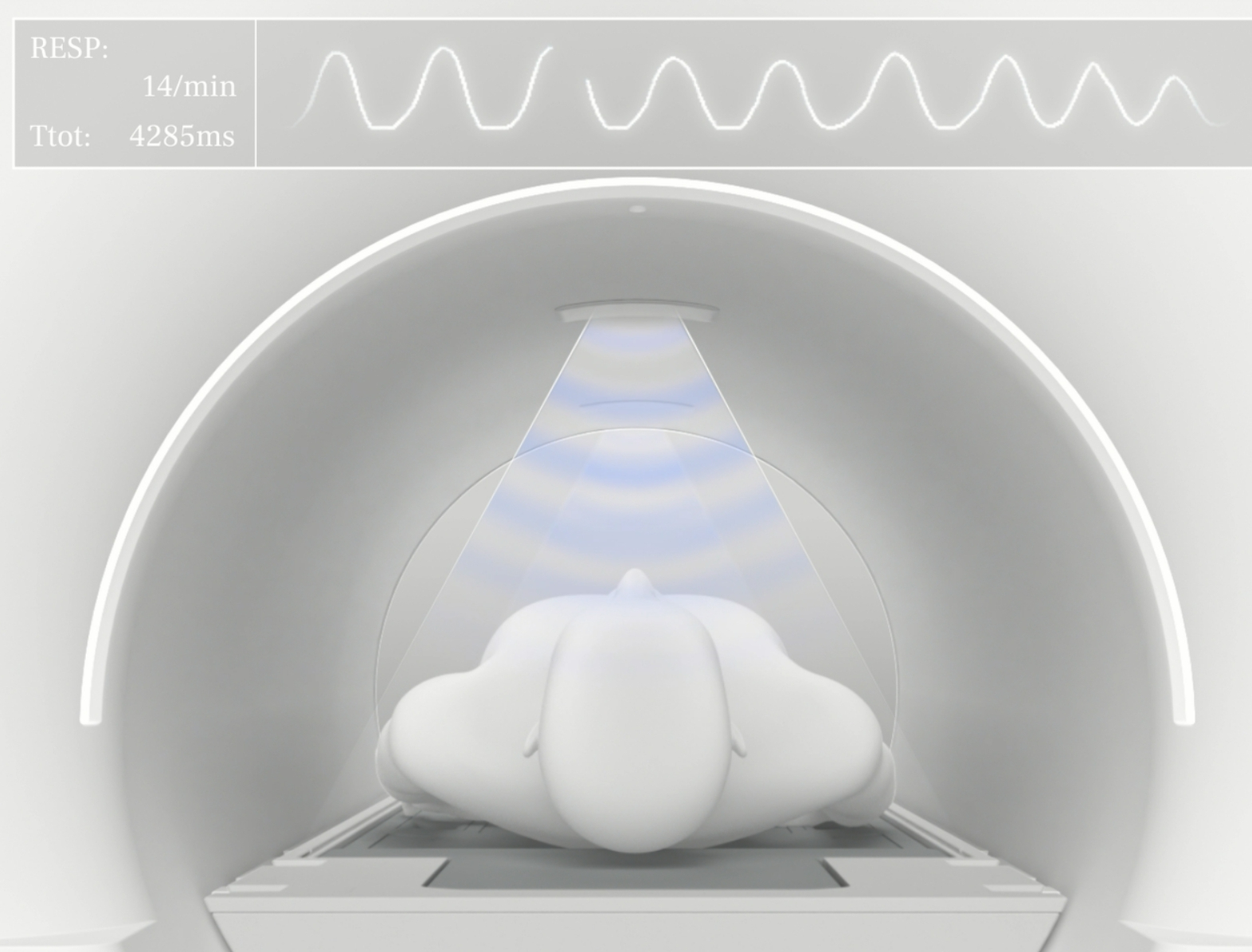
- maternal obesity – when excessive maternal weight makes accurate ultrasound evaluation difficult, MRI can provide a clearer picture of foetal structures;
- diagnosis of complex foetal defects, including defects of the brain, thoracic and abdominal organs, and congenital malformation syndromes. MRI is also invaluable in diagnosing complications resulting from intrauterine infections that can affect foetal development;
- disease history in the family – in situations where the mother suffers from diabetes, has had a miscarriage in the past, or the foetus’s siblings have been found to have congenital or genetic defects. In such cases, MRI can help identify similar problems in the developing foetus;
- MRI provides precise images required to accurately plan and carry out surgical interventions on the foetus, and allows doctors to prepare for possible complications and schedule surgeries as soon as the baby is born, especially in cases where a quick medical response is required;
- the need to terminate pregnancy when serious foetal abnormalities or placental pathologies (placenta previa, placenta increta or placenta percreta) are present;
- suspected conditions of the mother’s organs located within the abdominal cavity and within the pelvis minor;
- acute abdominal pain, which may be caused by appendicitis, gallstones or inflammatory bowel disease;
- emergency conditions such as suspected stroke, brain tumours or meningitis;
- diagnosing and monitoring conditions such as placental abruption or suspected foetal malformations.
How to prepare for an MRI during pregnancy?
Preparation for an MRI scan during pregnancy is not significantly different from standard preparation procedures for this examination, but requires special precautions.
It is important for the mother to consult her obstetrician and a radiology specialist before proceeding with the examination. All available diagnostic options should be discussed, and the potential risks and benefits of MRI should be assessed.
The patient should arrive for the examination in loose clothing free of metal parts and refrain from wearing jewellery, watches or hair clasps that could affect MRI images or pose a safety risk.
Can pregnant women be administered a contrast agent?
Due to the fact that it contains gadolinium – a metal that can cross the placenta, accumulate in the foetus and adversely affect its development – it is not recommended that pregnant women be administered a contrast agent. Examinations involving contrast agents are only performed in critical situations when the potential benefit to maternal health outweighs the potential risk to the foetus.
In this case, the duration of the examination is shortened to limit the foetal exposure to contrast as much as possible. After the examination, pregnant women are advised to drink plenty of fluids. By drinking plenty of fluids, the mother-to-be can speed up the process of excreting the contrast agent from the body, thus minimising potential risks to the developing foetus.
Although magnetic resonance imaging is generally considered safe in pregnancy, the decision to perform an MRI scan should always be made on a case-by-case basis by the doctor who takes into account the patient’s medical condition. Every medical procedure carries certain risks, so caution and careful analysis of the possible benefits and risks is essential. It is always crucial to strictly follow guidelines and discuss possible concerns with specialists to ensure optimal safety for both the mother and the developing foetus.
*ATTENTION! The information contained in this article is for informational purposes and is not a substitute for professional medical advice. Each case should be evaluated individually by a doctor. Consult with him or her before making any health decisions.